Improvement StoriesSecond Stage Labor:
Promoting Physiologic Pushing and Laboring Down Contributors:
Mary Kindle BSN, RNC, CPHQ
Marshe Remynse MSN, RN, FNP-BC
Beth Sangalli BSN, RNC
Jennifer Burhans MSN, RN 
Bronson Methodist
Health System
What did you set out to change or improve?
In 2010 Bronson Methodist Hospital agreed to participate in the Michigan Hospital Association Keystone OB Collaborative. One of the indicators for this initiative was management of second stage of labor, which included laboring down and non-directed, open glottis pushing. How did you change it? What new policy, process, or practice did you put in place?
A Certified Nurse Midwife (CNM) was recruited as our champion. The CNM along with a multidisciplinary team worked together to roll these evidence-based practices out to the staff. Education was provided to physicians and midwives via Grand Rounds. Evidence based journal articles were made available to providers and nursing staff. Education for the Labor and Delivery nurses was presented at staff meetings and other educational sessions. Conversations were initiated with staff during their shifts on Labor and Delivery regarding changes and evidence behind them. This gave them the opportunity to express concerns and ask questions. Evidence in the form of written articles and other nurses personal experiences using these practices could also be shared. Who was involved in making the change and what was each person’s role?
The CNM champion, Perinatal Clinical Nurse Specialist, Labor and Delivery managers, OB nurse educator and child-birth educator collaborated to provide education, mentoring and encourage grassroots support from both providers and nurses. How did you determine if the change worked? What data did you collect? How did you define “success”? How did you ensure your change didn’t have any unintended negative consequences?
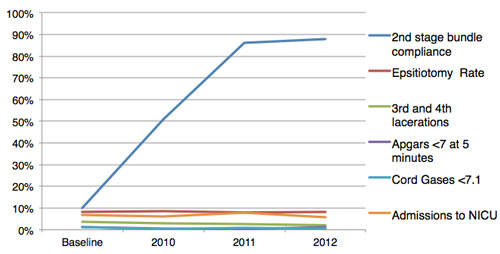
As part of the data collection for the MHA Collaborative, mother charts were audited for laboring down, positioning and non-directed pushing (second stage bundle) by designated Labor and Delivery nurses. Data regarding number of admissions to NICU, Cord gases less than 7.1 and Apgar score less than 7 at 5 minutes were collected to monitor for unintended consequences. The number of episiotomies and 3rd and 4th degree lacerations were monitored in addition to the indicators for the collaborative. What was the biggest barrier to making the change?
There was some resistance amongst providers regarding laboring down because of concerns that it would extend time of second stage as well as whether there were real benefits. While there was good evidence from the midwifery research, the evidence from the medical literature was somewhat mixed. Non-directed, open-glottis pushing was a difficult change for the nurses, providers and patients’ family members. The practice of breath holding and counting to ten was such an ingrained practice that staff and family members of the mothers were unsure of how to assist using the new practices. Nurses and providers were not convinced that the new techniques would be effective. How did you overcome that barrier?
As people began trying the techniques and saw success for themselves, the practice changes were slowly adopted by the majority of providers and nurses. Nursing was a strong advocate with resistant providers in encouraging them to allow the patients to labor down. Educating patient and family members during childbirth education classes and at the time of delivery about the new pushing techniques was also used. However, there continued to be some outliers who were never really convinced. Here is an example of our monitoring data to confirm we were making the change and sustaining it over time.
| Baseline | 2010 | 2011 | 2012 | 2nd stage bundle compliance | 10%
| 51%
| 86%
| 88%
| Episiotomy Rate | 8.4%
| 8.7%
| 8.0%
| 8.3%
| 3rd and 4th lacertations | 3.7%
| 2.9%
| 2.5%
| 2.1%
| Apgar <7 at 5 minutes | 1.4%
| 0.5%
| 0.3%
| 1.2%
| Cord Gases <7.1 | 1.4%
| 0.3%
| 0.9%
| 0.7%
| Admissions to NICU | 6.8% | 6.2% | 7.8% | 5.7% |
If you had one piece of advice for someone who wanted to make a similar change in their setting, what would you advise
Provider and staff nurse champions are the key to implementing a change such as this. Also, having a multidisciplinary team working together to develop a plan for the changes in practice is important. Building the support of a few key leaders and then having them share with their colleagues is vital.
|